How I Self-Diagnosed and Treated My Hypertrophic Cardiomyopathy
An often over-looked heart condition, basal septal hypertrophy was making me dizzy when I ran.
The skeptical cardiologist has been taking a beta-blocker, nebivolol, for the last seven years. Like all beta-blockers, nebivolol (brand name Bystolic), slows the heart rate and lowers the blood pressure, and can be used for cardiac rhythm problems (i.e. PVCs, PACs, VT, afib) and cardiomyopathies.
I put myself on the drug after diagnosing myself with a form of hypertrophic obstructive cardiomyopathy (HOCM) in 2015.
The treatment for exertional symptoms in patients with HOCM is typically a beta-blocker. Within a day of starting the nebivolol, I was able to run without chest pain or near-syncope.
Symptoms Developing During Exercise
I was about 2 years post extensive abdominal surgery for carcinoid tumors that were identified in my small intestine and was trying to get into better shape by running.
Shortly after starting the run, I would notice a tightness in my anterior chest associated with a sensation that I was going to pass out
When I felt this sensation, if I continued running or even slowed down it would worsen to the point that I felt compelled to stop and sit down on the sidewalk in order to avoid the embarrassment of passing out.
What I experienced, feeling very faint, is termed near-syncope. If I had continued to worsen and lost consciousness I would have "passed out" and fallen to the ground and this would be termed syncope. The chest tightness on exertion is classic for angina, a symptom of severely blocked coronary arteries.
An Abnormal Echocardiogram Read As Normal
I knew that the major causes of exertional syncope are cardiac: aortic stenosis and hypertrophic obstructive cardiomyopathy (HOCM) being the most common.
I had experienced chest tightness without the near-syncope with exercise in 2012 but at that time a stress echocardiogram was performed on me and was read as normal.
The apparently normal echo interpretation meant that I didn't have aortic stenosis which is much slower in onset and would likely not have been missed and/or developed in 3 years. The normal stress echo plus a subsequent coronary CT angiogram ruled out coronary artery blockages severe enough to cause my symptoms.
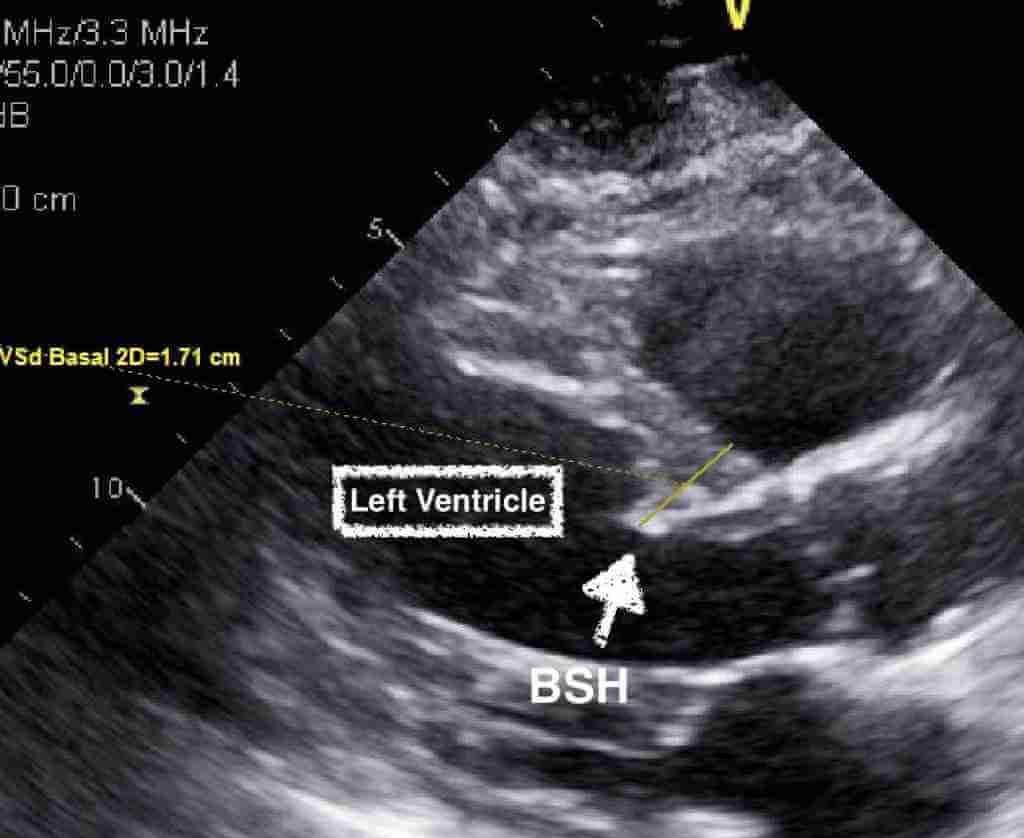
I went back and examined my echocardiogram in detail and noted that the basal portion of my ventricular septum bulged a little compared to the mid-portion. I reviewed the cardiac CT and this confirmed the basal septal thickening.
Neither the reader of the echocardiogram nor the reader of the cardiac CT made any note in their chart of the thickened area.
It is not uncommon for echocardiographic studies to be botched either by over or under diagnosis as I noted in an article entitled "Echocardiograms-Botched, Misread, or Overutilized." You can read about my dad’s heart murmur and his botched echocardiogram here and read about the dangers of undergoing shoddy, mobile cardiovascular screenings including echos here and here,
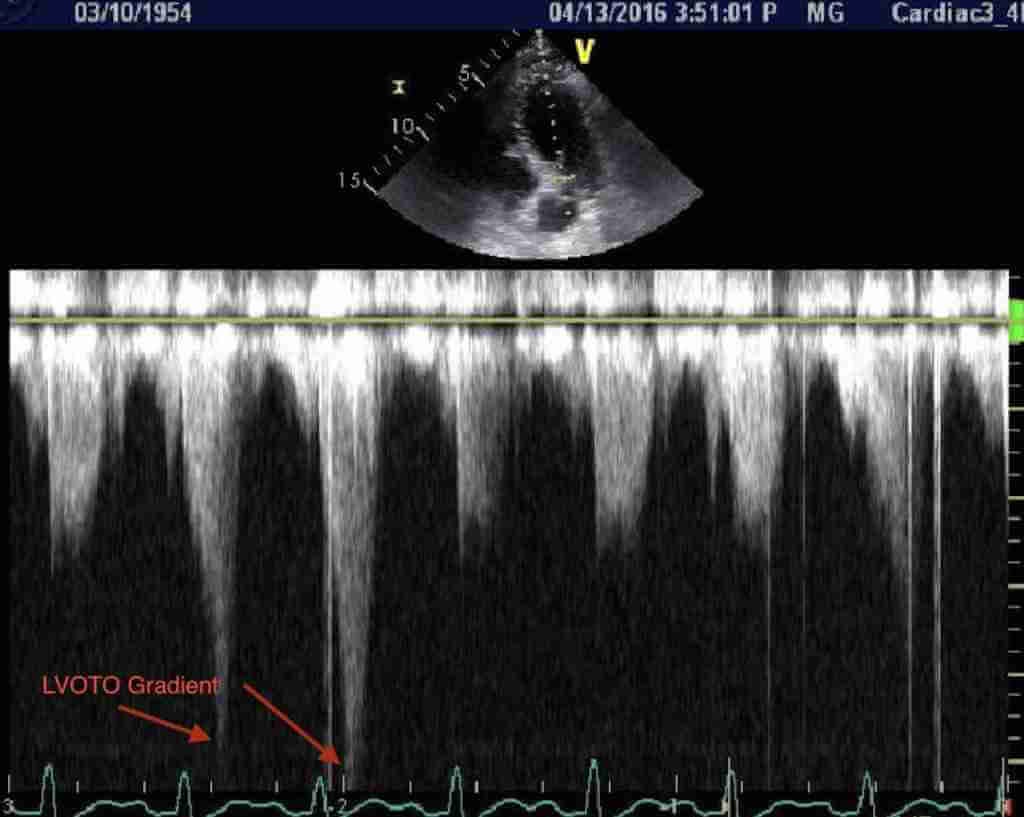
Ultimately, I had another stress echocardiogram performed on me. This time I informed the sonographer performing the test to pay special attention to precisely measuring the mid and basal portions of the ventricular septum segments and to measure the development of obstruction within the left ventricle by Doppler immediately post-stress.
This stress echocardiogram confirmed the diagnosis of hypertrophic obstructive cardiomyopathy with severe obstruction developing with exercise. This, then, was the reason for my symptoms.
Research and a Paper
Ironically, I wrote a paper on hypertensive hypertrophic cardiomyopathy of the elderly in 1988, long before I had any signs or symptoms of the disease.
After diagnosing my specific form of cardiomyopathy, I spent a lot of my free hours researching the condition as it was clear that it was under-recognized in the general cardiology community.
Mild thickening or protrusion of the basal ventricular septum was identified in 1969 and initially termed a "sigmoid septum." Initial studies suggested this was a benign finding related to hypertension and aging.
My research suggested otherwise and I decided to write an academic paper that would summarize the history of this entity, unify the diagnostic terminology, and make clinicians more aware of it.
After months and months of crawling through the peer review process with multiple revisions, it was finally published in 2017 in the journal, Echocardiography.
In my introduction, I give references for each of the 12 different terms that have been used in the imaging literature to describe this anatomic/echocardiographic finding.
Localized thickening of the basal portion of the ventricular septum has been identified by necropsy and imaging studies for decades, but there is no consensus on its significance and a remarkable lack of consistency in terminology. This anatomic finding has been termed:
localized hypertrophy of the upper portion of the ventricular septum
disproportionate ventricular septal hypertrophy,
disproportionate upper septal thickening (DUST)
sigmoid or sigmoid-shaped (interventricular) septum (typically felt to be benign)
localized septal hypertrophy,
basal ventricular septal hypertrophy
ventricular septal bulge
discrete upper septal thickening
upper septal knuckle/discrete upper septal thickening,
basal septal hypertrophy
sigmoid (sic) hypertrophy of the ventricular septum, characterized by the knob-like prominence of its basal subaortic segment
isolated hypertrophy of the basal septum
isolated basal septal hypertrophy (sigmoid septum) in elderly people
Unfortunately, although my paper has been cited 8 times since then, it hasn't had the earth-shattering (or at least echocardiographic earth-shattering) effects I had hoped for and I still see the diagnosis completely missed or given a benign-sounding name like "sigmoid septum."
However, I'm still running and not collapsing. And I'm still reading echos and findings lots of previously undiagnosed basal septal hypertrophy.
Disproportionately Yours,
-ACP





Titus,
I am not optimistic ML or AI will advance the field of echo interpretation. Attempts to automate the process of measuring the key parameter of ejection fraction using computer assistance have been going on for decades... and all have failed. Currently, there is a lot of buzz around measurement of strain as a better parameter for pump function of the heart. Clinical applicability is limited due to failure to visualize endocardium of the LV, something that is patient , machine and technician dependent and many other factors. A company Ultromics has developed a cloud-based AI platform which alleges superior interpretation . The studies are weak, biased and unlikely to be reproduced.
Garbage in creates garbage out and echo is just too operator dependent to be useful IMHO.
Dr P
JD,
Cardiologists utilize beta-blockers somewhat interchangeably for the indications I mentioned. We seek the most effective and well-tolerated type and dosage.
One area where they are not interchangeable is heart failure/cardiomyopathy/post MI where I utilize carvedilol or metoprolol succinate almost exclusively.
There are slight variations in beta-selectivity and alpha-selectivity among the various beta-blockers which play a roll in efficacy and tolerability.
Dr. P