Does Treating Sleep Apnea With CPAP Improve Cardiovascular Outcomes or Lower Risk of Atrial Fibrillation?
The sleep apnea industry would like you to believe that it does but high quality data show that CPAP is ineffective in improving cardiovascular outcomes for most individuals
Despite the widespread belief that obstructive sleep apnea (OSA) causes cardiovascular events like strokes and heart attacks, there is no good evidence that treating OSA lowers the risk of such cardiovascular outcomes.
Observational data showing that OSA is associated with cardiovascular outcomes like atrial fibrillation, stroke, CV death, and myocardial infarction have been utilized by the sleep apnea academic-industrial complex (in ways very similar to the omega-fatty acid (OMFA ) academic-industrial complex) to market the need for sleep apnea diagnosis and treatment.
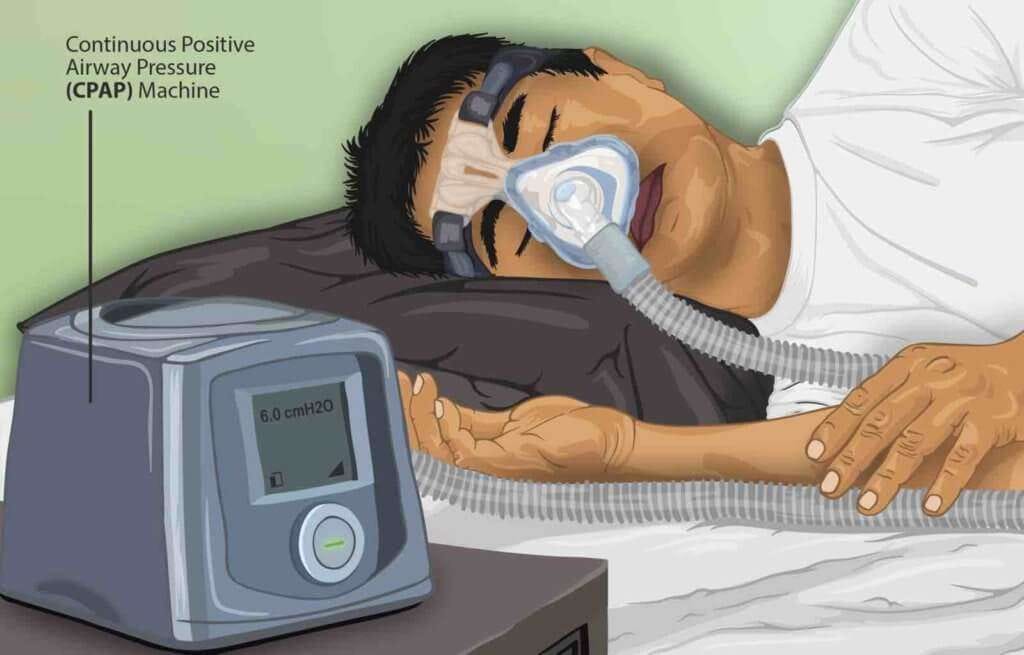
However, as we saw in the OMFA world, causality can only be proven with a randomized trial of effective therapy of the disease (given that there is no way to randomize patients to having OSA or not having it.) The most widely prescribed and effective therapy for OSA is continuous positive airway pressure (CPAP).
Healthy User Bias is a major confounder of most CPAP and all observational studies as noted at ClinicalCorrelat…
Keep reading with a 7-day free trial
Subscribe to The Skeptical Cardiologist to keep reading this post and get 7 days of free access to the full post archives.