Dealing With Symptoms That Develop While Taking Statin Drugs
Featuring Samson, Delilah* and the Nocebo Effect
The skeptical cardiologist wrote a long post in 2017 entitled "Do Statins Cause Memory Loss? The Science, The Media, The Statin-Denialist Cult, and The Nocebo Effect" which was updated in 2019.
If you'd rather not be bothered with the longish discussion in that post, complete with scientific references, the answer is no, statins don't cause memory loss.
The FDA added a warning to the statin patient information in 2012 based on a few case reports. Occasional reports of patients developing memory loss while taking a statin do not prove that statins are a significant cause of cognitive dysfunction.
Case reports of drug side effects have to be viewed in the context of all the other scientific studies indicating no consistent evidence of negative neurocognitive effects of the statins. We should be skeptical of case reports for several reasons:
First, patients receiving statins are at increased risk for memory loss because of associated risk factors for atherosclerosis and advancing age. A certain percentage of such patients are going to notice memory loss independent of any medications.
Second, the nocebo effect: If a patient taking a statin is told that the drug will cause a particular side effect, that patient will be more likely to notice and report that particular side effect.
Since I wrote about the nocebo effect, a wonderfully insightful trial has been published demonstrating very clearly how powerful it is.
Documenting the Nocebo Effect
The SAMSON trial enrolled 60 participants who had had statin side effects sufficiently severe to have abandoned statin therapy.
Participants received 12 1-month medication bottles, 4 containing atorvastatin 20 mg, 4 placebo, and 4 empty.
The statin was atorvastatin 20 mg film-coated (Ranbaxy). The bespoke placebo was manufactured with an identical appearance (GSTT Pharmaceuticals). Daily symptom intensity was measured using an app (scale 1-100). Researchers measured the “nocebo” ratio: the ratio of symptoms induced by taking statin that was also induced by taking placebo.
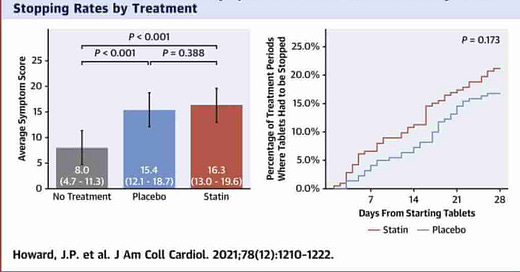
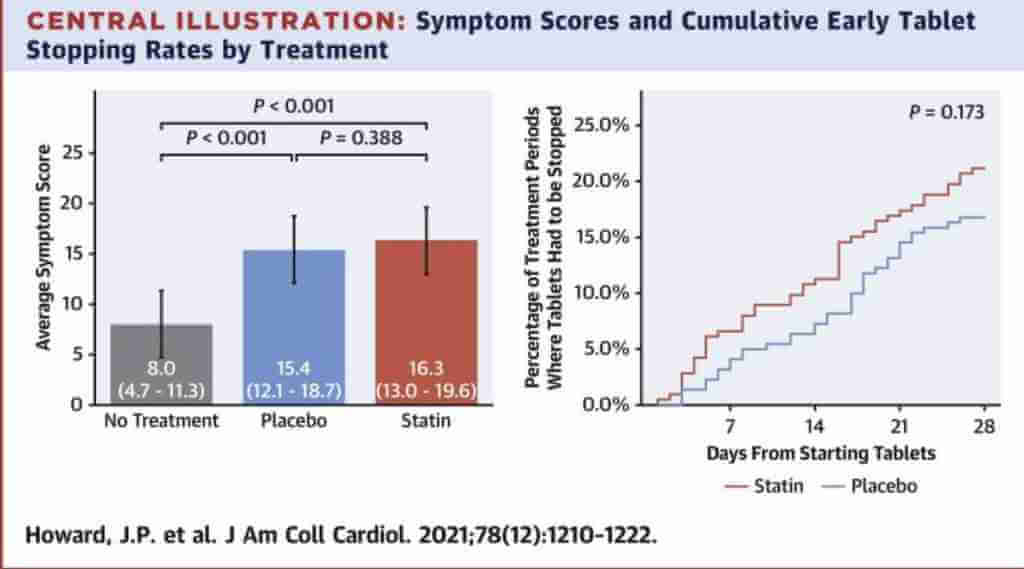
The study found that 90% of symptoms reported while taking statins were also reported while taking a placebo, and that people were just as likely to stop taking either due to side effects.
Stopping was no more frequent for statin than placebo (P = 0.173), and subsequent symptom relief was similar between statin and placebo.
Importantly at 6 months after the trial, 30 of 60 (50%) participants were back taking statins.
In a separate paper**, the authors list possible causes of these findings including:
‘Ever Present’ Chronic Background Symptoms
When patients are asked about symptoms on statins, they correctly describe them. Because of the prejudice that statins cause such symptoms, and the absence of formal documentatio,n of symptom intensity with and without statins, the symptoms are, understandably, attributed to the statins.
Intercurrent Conditions Inducing Symptoms
Even though these occur stochastically, patients and clinicians often conduct informal experiments, with disastrous consequences. When the symptoms are most intense, the statin is stopped, and the symptoms can only improve, termed regression to the mean (Morton & Torgerson, 2003). Conversely, the statin is only restarted when the symptoms have resolved, and therefore can only get worse. They therefore find a convincing association between starting and stopping statins and the onset and offset of symptoms. However, this association is purely an artifact of these experiments not having a preset schedule.
The Nocebo Effect
For reasons that are not clear, some people have developed a physical reaction from taking a tablet that they believe could be a statin. It is also not an imaginary symptom. It is just as real as the palpitations and sweating one would feel if threatened by an armed robber—there is a genuine biological response.
True Pharmacological Side Effect
This would become evident from the symptoms on statin being higher than those on placebo. SAMSON and StatinWISE suggest that this is a small proportion, even among patients who had to give up statins because of side effects.
In my experience, the most important factor in determining whether my patient experiences side effects on a statin is whether or not they have been told negative things about the drugs :
Sources of priming include reports from friends and family, media and internet coverage, and side effects listed in leaflets (that conventionally do not compare active with placebo) . A clinician responding to symptom reports by changing the dosage, frequency, or agent reinforces a patient’s belief that the statin was the cause of the symptom. SAMSON tested for this by having both no-tablet and placebo tablet arms, which reveals the expectation of side effects (ie, nocebo) to be the dominant contributor, because symptoms were much worse on placebo tablets than no tablets (P < 0.001), and no different between placebo and statin (P = 0.388). Furthermore, 10 participants who had to stop tablet months early managed, after discussion of their personalized results, to successfully restart statins.
I talk about this in detail in my prior post on the nocebo effect: "Steve Nissen*** wrote an eloquent article that accuses statin deniers of being an “internet-driven cult with deadly consequences":
“Statins have developed a bad reputation with the public, a phenomenon driven largely by proliferation on the Internet of bizarre and unscientific but seemingly persuasive criticism of these drugs. Typing the term statin benefits into a popular Internet search en- gine yields 655 000 results. A similar search using the term statin risks yields 3 530 000 results. One of the highest-ranking search results links to an article titled “The Grave Dangers of Statin Drugs—and the Surprising Benefits of Cholesterol”. We are losing the battle for the hearts and minds of our patients to Web sites developed by people with little or no scientific expertise, who often pedal “natural” or “drug-free” remedies for elevated cholesterol levels. These sites rely heavily on 2 arguments: statin denial, the proposition that cholesterol is not related to heart disease, and statin fear, the notion that lowering serum cholesterol levels will cause serious adverse effects, such as muscle or hepatic toxicity— or even worse, dementia.”
Dealing With Statin Side Effects In My Practice
After 30 years of practice, I’ve concluded that in any individual patient, it is possible for any drug to cause side effects. And, chances are good that if we don’t address the side effects the patient won’t take the medication.
Since statins are our most effective and best-tolerated weapon in the war against our biggest killer, it behooves both patients and physicians to have a high threshold for stopping them altogether. Having such a high threshold means filtering out the noise from attention-seeking media and the internet-driven denials cult thus minimizing the nocebo effect
If the side effect is significant I tell the patient to stop the statin and report to me how they feel after two to four weeks.***
If there is no improvement I have the patient resume the medication and we usually reach a consensus judgement that the side effect was not due to the medication.
If there is a significant improvement, I accept the possibility that the side effect could be from the drug. This doesn’t prove it, because it is entirely possible that the side effect resolved for other reasons coincidentally with stopping the statin. Muscle and joint aches are extremely common and they often randomly come and go.
When a patient tells me that they feel the rosuvastatin we started 4 weeks earlier is causing them to have more diarrhea or cough I inform them that there is no evidence that rosuvastatin causes diarrhea or cough more often than a placebo and there is no reason based on its chemistry to suspect it would. (Although I’m sure there is a forum somewhere on the internet where patients have reported this). If they accept my expert opinion and continue taking the drug we almost invariably find the symptom resolve on its own.
For all other symptoms, it is extremely unusual to see a return on rechallenge with statin and so we continue statin as a long-term therapy.
When a patient tells me that they feel the rosuvastatin we started 4 weeks earlier is causing them to have more diarrhea or cough I inform them that there is no evidence that rosuvastatin causes diarrhea more often than a placebo and has no reason based on its chemistry to suspect it would. (Although I’m sure there is a forum somewhere on the internet where patients have reported this). If they accept my expert opinion and continue taking the drug we almost invariably find the symptom resolve on its own.
When a patient tells me they believe they are having a side effect from the statin they are taking (and this applies to any medication they believe is causing them side effects), I take their concerns very seriously.
If the symptoms persist and the patient continues to believe it is due to the statin, we will go through the process I described above. And, since every patient is unique, it is possible that my patient is having a unique or idiosyncratic reaction to the statin that only occurs in one out of a million patients, and thus is impossible to determine causality.
Fortunately, since I first wrote about the nocebo effect, multiple very effective and safe alternatives to statin drugs have been approved which we can move to prescribing for lipid-lowering and ASCVD risk reduction in patients who are not able or willing to tolerate statins. These include ezetimibe, PCSK9 inhibitors, and bempedoic acid.
Antinocebonically Yours
-ACP
*I admit that I don't actually mention Delilah in this post. Some may accuse me of creating a click-bait headline but consider this tortured analogy: Samson's haircut by Delilah was an inert action (long hair doesn't make you stronger) that led to negative effects (weakness) and therefore is a great example of the nocebo effect!
**"Why Do I Get Side Effects? Personalized (N-of-1) Trials for Statin Intolerance and the Nocebo Effect" by James Philip Howard, Frances A. Wood, and Darrel P. Francis. This paper also discusses the 2021 STATIN-wise RCT which had similar findings to SAMSON
***Nissen has done extremely important research helping us better understand atherosclerosis and is known for being a patient advocate: calling out drug companies when they are promoting unsafe drugs.
****The authors of the SAMSON trial are critical of my approach and recommend one with a protocol that includes placebo pills. Unfortunately, placebo pills are not available to clinicians and such protocols are unrealistic in a busy clinical practice. They write:
The cues and informal experiments patients and clinicians use to test causation can paradoxically confirm a nonexistent association. This error is prevented by a scheduled, 3-armed, crossover trial containing no-tablet periods. Participating in such a protocol allows one-half of patients with reported side effects to successfully restart statins.
N.B. The British Heart Foundation published a nice article aimed at laypeople that summarizes Samson and features a patient who participated in the study.
For readers who seek an incredibly deep dive into statin-associated muscle symptoms (SAMS) check out this 2023 review article in the Journal of Clinical Lipidology
The portmanteau term drucebo effect has been proposed "to overcome the difficulties associated with measuring the nocebo effect, and the fact that its definition refers to inert compounds, rather than drugs." It is a combination of DRUg and plaCEBO or noCEBO and relates to the "beneficial or adverse effects of a drug, which result from expectation and are not pharmacologically caused by the drug."



I love your substack think you are a reasonable sensible person. I am 55 have a family history of high cholesterol from Mom and Dad ( dad has lipoprotein a) I was tested for the lpa at Dad’s heart doctor’s urging I don’t show high levels . My cholesterol was 297 total. I refused to take the statins for over a year. Watching my father and younger brother suffer with open heart surgery and clogging I decided to try the statins. I took crestor from April til mid July. My leg muscles felt so stiff it was difficult to walk. My hands ached like I had arthritis. My left outside tendon on my leg swelled up and was sore and painful. It still has not healed yet. My doctor put me on lipitor. After a month same symptoms. Long story short I asked for a calcium heart scan to even see if I needed to take the meds. My score was bad 297. So my cardiologist was able to give me Repatha which I self inject every 2 weeks. I have a little leg muscle tightness for few days after injection then I am fine. I am not a complainer about pain or medication as general rule. But I really could not tolerate the statins. I am glad you like my doctor listen and try to help find a reasonable solution. This medication is life saving and I hope will keep me off the operating table for many years. Keep up the informative articles on heart disease which has been so hard on my family.
does this author have a point in that ARR from statins is small? https://pubmed.ncbi.nlm.nih.gov/35285850/
I assume this article is quackery, but thought I would ask: https://cardiacos.net/wp-content/uploads/2019/04/2015-Statins-stimulate-atherosclerosis-and-heart-failure-pharmacological-mechanisms.pdf