COVID-19, Past, Present, and Future: The 2022 Perspective
What was clear became murky and what was murky has become clear.
Since early 2020, the COVID-19 pandemic has been at the forefront of the world's consciousness and the skeptical cardiologist has written extensively on aspects of the pandemic that could be clarified. Looking back on 2022, much progress was made toward achieving a "new normal" in dealing with COVID-19 but many questions and much controversy remain.
What was clear early on became murky and what was murky has become clear. Let's look back at the year in COVID-19 through the eyes of a skeptical physician and patient who made difficult decisions regarding boosters, masking, and oral treatments.
Paxlovid
In January of 2022, I described in detail the first new effective oral therapy for COVID-19, Paxlovid.
Paxlovid looks to be very effective. In a randomized controlled trial in non-hospitalized unvaccinated symptomatic patients with confirmed SARS-CoV-2 it reduced the proportion of patients with COVID-19 related hospitalization or death from any cause by 88% compared to placebo among patients treated within five days of symptom onset.
I emphasized the need for patients, especially those on cardiac medications to check for drug-drug interactions in an article entitled "The New COVID-19 Pill, Paxlovid, Interacts with Many Medications: Cardiac Patients Take Note.
Ironically, a family member was just diagnosed with COVID-19 and was prescribed Paxlovid. When she texted me I advised her to check for drug-drug interactions. She texted me that she had already started taking it and that her doctor knew all of her medications.
I said "I know you have a lot of trust in your doctor but even the best doctors can make mistakes. Take a few minutes to make sure none of your drugs are on this checklist."
After reviewing her medications, three were on the checklist which had significant interactions with Paxlovid.
No matter how great or meticulous you feel your doctor is, I highly recommend checking your medications against this checklist before starting Paxlovid. The good doctor will thank you for your diligence.
The New Normal
In January 2022, given the emergence of an effective oral agent and vaccines and the overall decline in deaths and hospitalizations related to COVID-19 with the newer variants, I wrote "How to Achieve The ‘New Normal” life With COVID-19." This summarized publications which encouraged recognition that COVID-19 is here to stay and will not be eradicated.The SARS-CoV-2 virus should be viewed in the same category as seasonal influenza and other respiratory viruses.
To reduce COVID-19 transmission, achieve and sustain a “new normal,” and preempt future emergencies, the nation needs to build and sustain a greatly improved public health infrastructure, including a comprehensive, permanently funded system for testing, surveillance, and mitigation measures that does not currently exist
The mitigation measures discussed included masks, improved testing and surveillance, and upgrades to ventilation and air filtration systems.
Since then, it appears that most of the US (and President Biden) have accepted this new normal. Masking of any kind is no longer required even in airports or on airplane flights. Those who are particularly concerned about their risks of catching COVID-19 can wear masks as they see fit.
I have seen little progress in ventilation and air filtration.
The Boosters
In March, 2022, the FDA and CDC authorized the Pfizer and Moderna vaccines for the second booster in adults >50 years of age.
I reviewed my angst-ridden decision-making on the 4th jab in a post. Briefly, I am >65 years of age without other risk factors for severe COVID-19 (I have asthma and hypertension but don't consider these risk enhancers). I received an initial set of Pfizer shots in January of 2021 as soon as they were authorized and I jumped the gun on getting a Pfizer booster in August of 2021. I had upcoming inpatient hospital duties beginning April 18, 2022.
Ultimately, I decided to get the "4th jab" and described the experience in detail in The Second Booster is Under My Delt: Mixing and Matching, Side Effects, and Risk Calculations
At that time I felt "the fourth booster is definitely not needed for those under age 50 years with no other risk factors. For those over age 80 years or those who are immunocompromised it is highly recommended."
I also noted that "for the rest of us this becomes a highly individualized decision. As I indicated I would not have gotten it if I was not looking at potential high exposure situations. I would not have gotten it if I had had significant side effects from prior COVID vaccinations. One reader commented on experiencing frequent symptomatic PVCs after his third injection. That would have steered me away from a fourth."
Ironically, about 5 days after writing that piece I developed significant symptoms that lasted about a week. I haven't written about these previously. I developed intermittent chest tightness, generalized weakness and exercise intolerance. I considered the possibility that this might be myocarditis related to the vaccination but this is unheard of in my age range. I considered getting an ECG and a troponin level but did not. I'm not sure what these symptoms were from but I now factor that episode into my decision-making for future vaccinations.
Contracting COVID-19
After receiving the 4th jab my wife and I "loosened up" and stopped wearing masks except in rare cases. I realized I was increasing my chances of catching COVID-19 but given my super quadrivaccinated state and the seeming inevitability of avoiding the illness without living a cloistered and/or masked existence, I felt ready for my date with SARS-CoV-2.
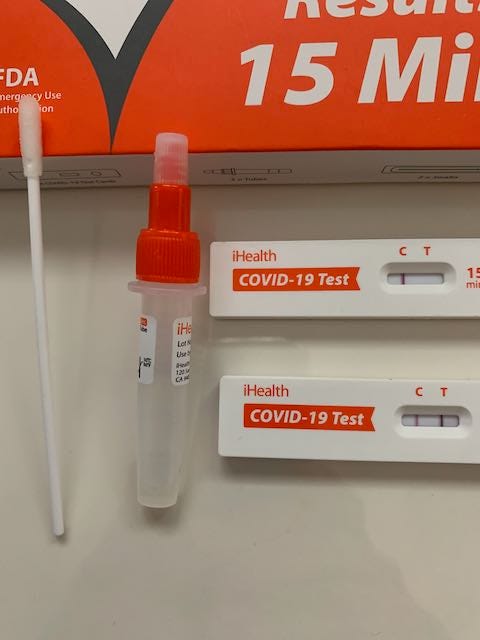
Two days after attending an indoor medical gathering I began feeling very fatigued. The fatigue continued the next day accompanied by a mild scratchiness in my upper airway. the weakness and malaise became progressively worse as the day wore on. By mid-day I tried to take a walk and after two blocks was exhausted. I took a COVID rapid antigen test which was negative.
The next day, I awoke at 3 AM with intense sneezing and nasal congestion which intensified over the next hour and became associated with a particularly nasty headache. I took 30 mg of the decongestant pseudophed, a Zicam tablet, my nasal steroid inhaler and ibuprofen. I couldn't sleep so I watched an episode of Better Call Saul. I retested myself again (15 hours after my initial negative test) for COVID and this time it was positive.
I described in detail my decision to take Paxlovid and how symptoms improved rapidly after taking it here along with the process of starting and stopping the isolation clock here.
Paxlovid Rebound
When I contracted COVID-19 in early May I was able to begin taking the antiviral medication within an hour of a positive home antigen test. I felt like within 12 hours of starting the medication my symptoms improved and during the 5 days of taking it I was progressively better each day.
Two days after stopping the Paxlovid I felt very good in the morning and rode my bike for 40 minutes. However, in the afternoon I began feeling anxious and worried for no apparent reason.
Subsequently, I redeveloped all the symptoms I had initially including fatigue, runny nose, cough, headache and weakness. Worsened symptoms continued through day 15 and then I began a slow steady improvement.
I discussed these rebound symptoms in detail here, noting that there were many cases and many unanswered questions. Rebound symptoms after COVID-19 occur in 1/3 of patients not taking COVID-19 but there are still many unanswered questions.
In particular, although the CDC recommends against repeat rounds of Paxlovid, many physicians are prescribing a second 5-day treatment. We also don't know if Paxlovid reduces the risk of long COVID. (And we don't know if long COVID is worse than prolonged symptoms after other causes of upper respiratory infection like influenza.)
Prolonged symptoms. I had lingering symptoms after my date with COVID-19 for about 6 weeks. From week 2 to 4 if I drank any alcohol at all I felt very weak and tired for 24 to 48 hours. This alcohol intolerance post-COVID has been described by others. My case would not fit WHO criteria for long COVID (>3 months.). My cardiorespiratory fitness was quite slow to improve and I watched my max V02 drop about 10% from 36 to 33. After 6 months, I’m almost back to my pre-COVID fitness levels.
Current Controversies Regarding COVID-19
My discussion of rebound in June of 2022 was my last post on COVID-19 on the skeptical cardiologist. I've come very close to writing several posts but concern about wading into areas of extreme controversy and uncertainty has stopped me.
-The Bivalent Booster. I am ambivalent about the bivalent booster. It was approved without a randomized controlled trial in humans. The observational data showing its efficacy in fully vaccinated individuals is weak. Given my quadrivaccinated state and my COVID-19 infection earlier this year along with the episode I had after my last booster I am holding off on getting the new bivalent booster until better data is released. For a good, detailed discussion of this check out This Week in Virology's You Tube video with Dr. Paul Offit (inventor of the rotavirus vaccine and pro-vaccine advocate.)
-Myocarditis. The issue of myocarditis in younger males who receive the boosters has been on my mind. Males <30 years are at an increased risk although most cases are mild and absolute risk is very low. However, because their risk (especially if previously vaccinated) of any serious complication of COVID-19 is incredibly low it is hard to know if the benefits outweigh the risks. I recommended my 29-year-old son (trivaccinated and previously COVID-infected) not get the bivalent booster.
Based on the discussion above it is clear to me that colleges should not be mandating bivalent boosters for students.
-Masks and Masking. Much has been made of a study that showed surgical masks were non-inferior to N-95s. This study only looked at healthcare workers during their time at work. It doesn't inform our decision on wearing a particular mask at other times. I'm still wearing an N-95 on airplane flights. On the other hand, UCSF oncologist and epidemiologist Vinay Prasad feels we are delusional to wear them at any time (see here.) Vinay and other authorities I respect also strongly feel there is no place for masking children in school.
I follow scientists/physicians on both sides of the COVID-19 issues and try to make my own independent, unbiased analyses of these thorny issues. Science is here to make the murky clear; to make the uncertain certain. The true scientist readily admits and often relishes uncertainty. Because SARS-CoV-2 is a rapidly evolving target and our tools to combat it are rapidly evolving, the murkiness is likely to dominate for some time but hopefully, our public health officials will be open and honest about what is certain and what is uncertain.
Clearly Yours,
-ACP




Gerry,
Thanks for your detailed and informed comment.
Re: "Recent evidence, however, supports use of the bivalent booster(s) for improving response to serious illness, hospitalization and death." The recently published evidence is all observational. Because those who choose bivalent boosters early will differ significantly from those who don't in many areas (including COVID-19 mitigations measures) I am not convinced by the modest effectiveness shown. But if I were higher risk I might still choose to get the vaccine. I don't counsel patients who are over age 65 or with risk factors against it.
Re "there are some clinics now recognizing Long COVID at 8 weeks, or even shorter intervals from onset, so falling to the WHO criteria isn't necessarily certain."
I agree this is happening and will definitely increase the number of patients identified with long COVID. I don't know if this is good or bad.
Re "On the issue of myocarditis/pericarditis, the interval you describe from your previous booster to the last booster seems inconsistent with the spate of myocarditis cases seen, and associated with (without true causation) mRNA boosters. It's been repeatedly noted that the incidence of myocarditis from infection is much higher than from vaccination. It's not impossible; I'd have wanted the ECG and troponin, personally, but the course would likely have been the same, save an abnormal result from either test would have landed you in the hospital."
Agree on the interval being too long. I did take AliveCor readings during this time to see if I was having PVCs. I wasn't. I also attempted a 12 lead using my Apple Watch. And I had a normal hs-CRP. If I had had PVCs, worrisome ECG changes or an elevated CRP I would have called another cardiologist gotten the trop and real ECG.
Dr. P
I had the bivalent vaccine this autumn to have another booster - and I had Covid (presumably Omicron) in June this year (after I got sloppy about wearing masks). After having had the virus I felt safer for the summer, although I continued to use face masks in supermarkets and in many other shops. Since having the booster I hardly use masks at all, and I’d say that this is because so few other people use them now. I would certainly admit to having been an advocate of face masks; what’s more, I read a number of articles on a medical website which were positive about the value of wearing them. However, even if I hadn’t read them, I’d have used some face covering or other - I wore a buff stuffed with a folded tea-towel while shopping for groceries in the first year of the pandemic.