A Primer on Atrial Fibrillation
Causes, treatments, stroke prevention, home monitoring and enlightened medical management
Atrial fibrillation occurs when the normal, regular, synchronous action of the upper chambers of the heart becomes chaotic, rapid, and inefficient.
Some who go into atrial fibrillation know it right away because they feel bad-they feel what we doctors term palpitations: a sensation that their heart is beating rapidly or irregularly (like a fluttering.) They may have other symptoms associated with this such as dizziness, chest pain, anxiousness or shortness of breath.
Many, however, go into atrial fibrillation and are not aware of it; in other words, they are asymptomatic.
For those who are asymptomatic, the first symptom felt may be due to a stroke from a clot developing in the (now dysfunctional) left atrium, or upper chamber of the heart, dislodging and going down an artery to the brain.
For others, especially if the heart rate is high, heart failure may develop, causing shortness of breath and prompting medical evaluation.
It is natural to wonder "Why Did I Go Into Atrial Fibrillation?" For some individual cases, specific triggers can be identified but for many, we never identify a particular cause.
For most patients persistently in atrial fibrillation, I recommend utilizing a combination of medications and cardioversions to restore the normal rhythm (normal sinus rhythm.) This is termed a "rhythm" management strategy. For decades we did not have solid evidence supporting this strategy over a "rate" strategy." A rate strategy is a conservative approach in which the patient is left to permanently be in atrial fibrillation but heart rate and stroke risk are controlled by medications.
I discussed in detail why I recommended the rhythm strategy in "Why I Favor The Restoration and Maintenance of Sinus Rhythm For Most Patients With Atrial Fibrillation." Since I wrote that stronger evidence has emerged supporting this position beginning with the 2020 Eastnet-AF trial I discuss below.
Whether you choose a rhythm or a rate strategy, the second major decision for AF patients is whether to take an anticoagulant to reduce the risk of atrial clot formation and resulting stroke. A good starting point for this discussion is "Blood Thinners (Oral Anticoagulants) For Atrial Fibrillation: Who Should Take Them and Which One To Take."
Diagnosing Atrial fibrillation
Atrial fibrillation is identified in myriad ways. Some patients feel very sick when they first go into it and end up in the emergency room. Others note only the marked increase or irregularity in their heartbeat and end up diagnosed by ECG in a doctor's office. An irregular pulse or heartbeat can be detected by many wearables and home BP devices which may alert users to the possibility of atrial fibrillation.
You can even take your own pulse and prevent a stroke by recognizing the characteristic “irregularly irregular” rhythm of atrial fibrillation.
There are thousands of patients now with permanent pacemakers and implanted defibrillators, devices that continuously monitor the heart rhythm. Brief, transient, and silent episodes of AF are often detected by these devices. Such episodes of "subclinical" atrial fibrillation are regularly detected with long-term monitors and loop recorders. I discuss current uncertainty around the optimal treatment of subclinical atrial fibrillation in "Subclinical Atrial Fibrillation: Seek and Ye shall Find, But What Then?"
Sometimes strokes present in unusual ways, like the inability to differentiate a spade from a diamond when playing bridge (described in TIAs and silent atrial fibrillation.) and afib can be the cause.
Using Personal ECG Devices To Diagnose Atrial Fibrillation
I've written extensively on the value of personal ECG devices to detect and monitor atrial fibrillation. There are two that I have considerable patient experience with and highly recommend:
AliveCor's Kardia
Using a Smart Phone Device and App To Monitor Your Pulse for Atrial Fibrillation (AliveCor)
AliveCor Is Now Kardia and It Works Well At Identifying Atrial Fibrillation At Home And In Office
2. Apple Watch 4 and higher
Apple Watch posts (here, here and here)
Devices/Apps I do not recommend for AF detection
Do NOT Rely on AF Detect Smartphone App To Diagnose Atrial fibrillation
Stroke Risk and Stroke Prevention
The most serious adverse consequence of having atrial fibrillation is stroke. Since we have safe and effective ways of preventing afib-related stroke with oral anticoagulant drugs (blood thinners), a major decision for the newly diagnosed patient with atrial fibrillation is “should I take a blood thinner?”
To answer this question the afibber should engage in a lengthy discussion with his/her health-care provider which results in a shared and informed decision. Such discussion must cover your risk of stroke, the benefits of blood thinners in preventing stroke, the bleeding risks of blood thinners, and the pros and cons of the various anticoagulants available to prevent stroke.
As background for these physician discussions, I highly recommend reading my post on "Which Patients Should Take Blood Thinners" which discusses stroke risk, anticoagulant risk, and the lack of efficacy of aspirin in this area.
Estimating Stroke Risk in Patients With Atrial Fibrillation You can estimate your stroke risk using an app that utilizes the CHAD2DS2-VASc score. I prefer to call the Lip score. This post was written in 2015 but the CHADS2 score is still the primary tool for assessing afib related stroke risk.
Why Does the TV Tell Me Xarelto Is A BAD Drug? Anticoagulant drugs that prevent the bad clots that cause stroke also increase bleeding risk. A bleeding complication is not a valid reason to sue the manufacturer. The lawsuits are strictly a money-making tactic for sleazy lawyers.
All patients with afib do not need anticoagulant therapy chronically. For some, we offer a pill-in-the-pocket approach, something I've touched on a few times on my blog.
Procedural alternatives to anticoagulant therapy have been developed including closure or obliteration of the left atrial appendage at the time of open heart surgery and closure using a catheter-based technology without surgery (left atrial appendage occlusion.) I have only referred rare patients for the FDA-approved catheter-based closure devices. For a good discussion on this area see Dr. Mandrola's article entitled "Left atrial appendage occlusion should be offered only to select atrial fibrillation patients."
Treatment Of Atrial Fibrillation
Lifestyle Changes
Eight Lifestyle Changes to Prevent Atrial Fibrillation
-Obesity.
How Obesity Causes Atrial Fibrillation in Fat Sheep and how Losing Weight can reduce the recurrence of atrial fibrillation.
More recently we have solid evidence that sustained weight reduction can significantly reduce the recurrence of AF from the Australian LEGACY study
-Alcohol.
Acute and Chronic Influences of Alcohol on Atrial Fibrillation
The alcohol AF trial published in NEJM showed abstinence from alcohol significantly reduced symptomatic episodes and hospitalizations for AF
-Fish Oil Supplements
Omega-3 Fatty Acids, Fish Oil Supplements and the Risk of Atrial Fibrillation discussed evidence that high-dose omega-3 supplements may cause atrial fibrillation.
-Exercise.
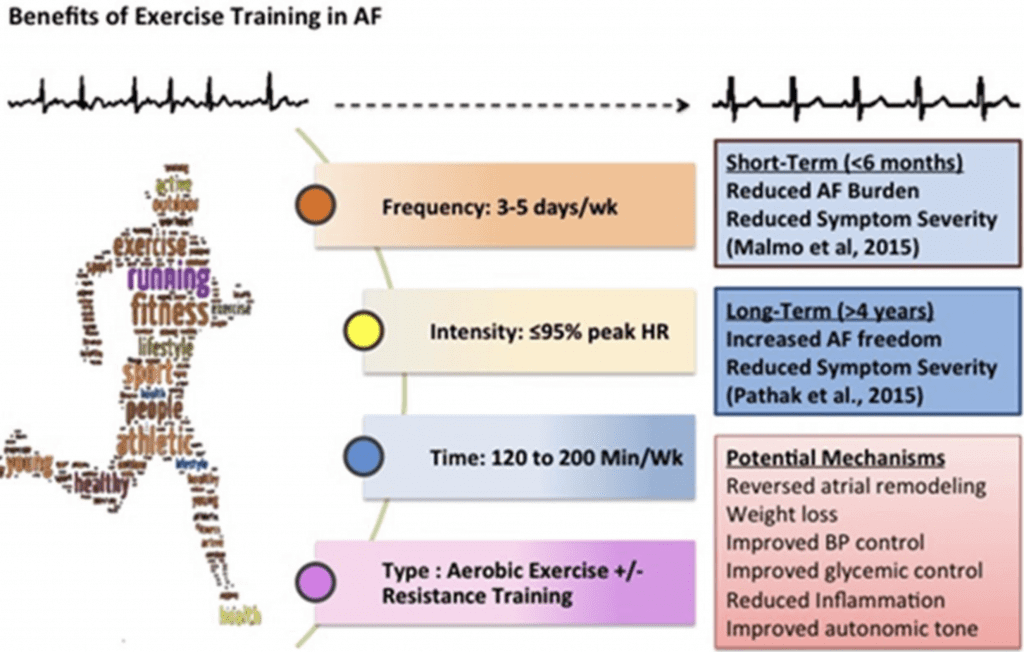
The most compelling evidence for the independent role of exercise in reducing AF comes from a Norwegian study of 51 patients with AF who were randomized either to aerobic interval training (AIT) or to their regular exercise habits. The exercise arm had a lower burden of Afib
Drug Therapy: Rate Control and Anticoagulation
Foxglove Equipoise. When William Withering began treating patients suffering from dropsy in 1775 with various preparations of the foxglove plant he wasn't sure if he would help or hurt them. After 240 years of treatment, we are still unsure if the drug obtained from foxglove is useful.
Should Digoxin Still Be Used in Atrial Fibrillation? The answer is it still has a minimal role in chronic outpatient therapy. In hospitalized patients we use it frequently intravenously to aid in slowing heart rate in hypotensive patients with rapid afib.
Drug Therapy: Antiarrhythmic Drugs for Maintenance of Sinus Rhythm
If lifestyle changes alone can't control atrial fibrillation, I am an advocate of enlightened use of medications (antiarrhythmic medications or AADs) that can safely restore and maintain the normal sinus rhythm long term.
The most recent study supporting drug therapy for suppressing atrial fibrillation, EAST-NET AF
My three-part series on "enlightened medical management of AF":
Part I: Amiodarone. Kardia and Cardioversions
Part II: The Pill-in-Pocket Approach
Part III: Flecainide for Chronic AF Suppression
There are other medications one can utilize for maintenance of sinus rhythm but I utilize them much less commonly than amiodarone and flecainide.
I discuss sotalol (Betapace) and beta-blockers here. Dofetilide (Tikosyn) is another alternative for the suppression of atrial fibrillation. Both of these drugs should be started in the hospital with the patient on an ECG monitor for 72 hours to monitor for ventricular tachycardia and QT prolongation.
I don't recommend Multaq (aka amiodarone light) and have a post pending on this topic.
Cardioversion and Ablation
We can shock (cardiovert) the heart back to normal rhythm with little risk and a very high success rate when performed by experienced and enlightened cardiologists. Keeping the rhythm normal after successful cardioversion is a bigger challenge (see above) and when medications and lifestyle changes fail an invasive procedure (ablation) is an option for some patients. Ablation should not be considered a cure for AF as recurrence is common and successful ablation has not been shown to lower stroke risk thus anticoagulants are still recommended lifelong after the procedure.
Cardioversion: How Many Times Can You Shock The Heart?
Ablation: Cautionary Words From Dr. John Mandrola and The Wisdom of a Team Approach
Ablation For Atrial Fibrillation: One Patient's Experience
Antifibrillatorily Yours,
-ACP





Gerry,
It has been a fascinating journey with afib since I started my cardiology training in 1984.
Once studies came out showing the superiority of warfarin over aspirin preventing stroke in afib I gave lots of talks (paid for by DuPont, the maker of Coumadin) on anticoagulation and how the new-fangled INR was superior to measuring PT alone. This was, of course, before I became the skeptical cardiologist and declined Pharma gifts/money/talks in order to maintain my unbiased status.
Mandrola recognizes the value of AFIB ablation for select patients, the limited efficacy and the complications but thankfully is not a gungho enthusiast. Most recently on TWIC he described how there are multiple white areas in the brain in patients who have undergone ablation, presumably micro embolic events, significance TBD.
Dr. P
Chip,
I have many patients who have only had one episode of atrial fibrillation. Typically this is a patient who had an unusual event that caused the atrial fibrillation.
I have one patient, for example, who had an episode of atrial fibrillation 15 years ago at a time when he had acute pericarditis. The pericarditis has not recurred and neither has the atrial fibrillation.
Some patients have their first episode of AFIB at the time of a severe pulmonary infection and have not had recurrent spells for decades. Others might have it at a time of profound hyperthyroidism that is corrected and not recur. About 1/3 of patients undergoing open heart surgery develop atrial fibrillation and recurrence rate is low.
I wish we had a good category name for the "one and done" fibber. And I wish we had good studies informing how best to manage anticoagulation in this group.
Dr. P